VISION DEFECT SURGERY
It is today legitimate to get rid of any type of optic correction.
Refractive surgery is now fully efficient and safe with more than 20 years follow-up, and well-established rules. In France more than 150 000 laser procedures are performed annually, specifically adapted to the particular morphology of each cornea – whether to its curvature, thickness, or its micro-irregularities (also called aberrations).
I personally had refractive surgery performed on my eyes 15 years ago for my biggest happiness, and can still see at far and near uncorrected.
All refractive errors can have a surgical correction, but not all candidates are operable. Surgical final decision is based on precise patient selection criteria, which will help choosing the most appropriate procedure, on a case-by-case basis. The therapeutic goal of refractive surgery can in no way be aesthetic; its sole purpose is to treat all forms of visual impairment.
Your vision is so precious. You need to know and trust the surgeon who will take care of such a valuable good.


THE TWO STEPS IN THE PREOPERATIVE CONSULTATION
Contact lens removal is mandatory for both steps: 48 hours prior to consultation in case of soft contact lenses, 1 month in case of rigid contact (it is possible to temporarily replace them by soft ones which will be removed 48 hours before the consultation).
Initial evaluation
The initial evaluation is performed in my office (61 rue de Rennes – 75006 Paris).
In a majority of patients pupil dilation is required, which prohibit driving or cycling during two hours.
Preoperative consultation is based on a complete exam. It includes of course refraction measurement in order to accurately quantify the refractive error and biomicroscopy of the anterior segment of the eye where surgery takes place. It also evaluates the quality of ocular surface and tends to eliminate any eventual concomitant ocular pathology, which could reduce the benefit of an eventual refractive surgery.
It includes several additional tests including conventional corneal topography, which visualizes the corneal architecture and its refractive power point by point, and pachymetry, which measures corneal thickness in the center and in the periphery. Particular, asymmetric and/or thin corneas can thus contraindicate, absolutely or relatively, refractive surgery.
Personalized preoperative testing
The second step is performed at Clinique de la Vision (131 rue de l’Université – 75007 Paris).
This second step is mandatory to validate surgical feasibility regarding safety strict criteria. Surgery cannot be performed unfortunately on all candidates. Some patients cannot have surgery at all; some are only eligible for a limited amount of procedures. If safety criteria are matched, the second step allows the choice of the most appropriate surgical procedure, as well as the technical protocol, which both ensure maximal postoperative satisfaction.
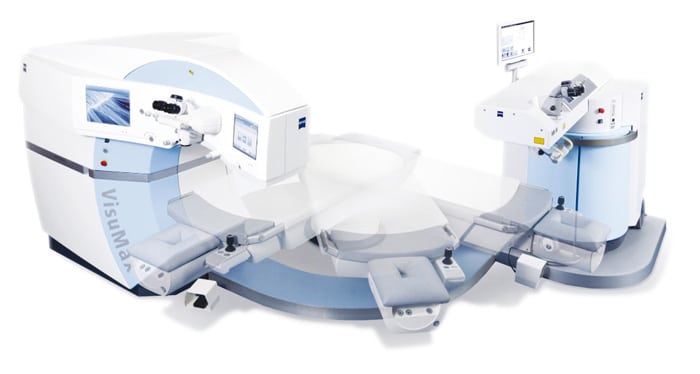
Tests are performed with ultramodern, sophisticated and regularly upgraded and/or renewed machines. Pupillometry measures pupillary diameter in mesopic darkness mesopic; it helps choosing the treatment protocol in order to minimize or eliminate any postoperative halo or glare. Elevation topography precisely analyses both anterior and posterior corneal curvatures and sometimes allows infra clinic corneal abnormalities that contraindicate excimer laser surgery. The anterior segment OCT (Optic Coherence Tomography) captures a tridimensional map of its anatomy and takes several measurements that will guide the surgical protocol (corneal thickness, anterior chamber depth, white to white ocular diameter, and so on). Aberrometry and wavefront analysis measure with microscopic accuracy, point by point, the entire refractive error of the eye, from the cornea to the retina; These measurements allow taking a biometric print of the eye that will be treated on a customized basis, dramatically enhancing thus the level as well as the quality of post operative result.
